Retina Treatments
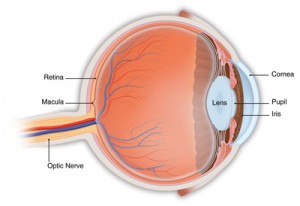
The retina is a thin layer of tissue on the inside back wall of your eye, containing millions of light-sensitive cells and other nerve cells that receive and organize visual information. Your retina sends this information to the brain through your optic nerve, enabling you to see.
Retinal diseases can affect the area of the retina that serves your central vision (the macula and the fovea at the center of the macula). Many retinal diseases share common symptoms and treatments, but each has unique characteristics. The goal of retinal disease treatments is to stop or slow disease progression and preserve, improve or restore vision.
Pepose Vision is a retina specialist and a leader nationwide in the research, diagnosis and treatment of retinal diseases.

How do I know if I have a retinal disease?
Retinal disorders may cause symptoms such as blurred vision, floaters (usually fine objects that appear as debris obscuring the visual image), and flashes of light. However, many conditions affecting the retina do not cause noticeable symptoms in the early stages, but may lead to irreversible and sometimes severe loss of vision. Symptoms may indicate a disorder limited to the eye or may be related to a systemic condition, such as diabetes, high blood pressure, cardiovascular disease (“narrowing of the arteries”), autoimmune diseases, metabolic disorders, blood infections, and certain types of cancers.
If you have diabetes or certain other medical or eye conditions, your primary medical doctor or comprehensive ophthalmologist can help you to determine when and how often to see a retina specialist.
The diagnosis and monitoring of retinal diseases requires a complete eye examination where the pupils are dilated with eye drops. You may experience a temporary change in vision and sensitivity to light, so you may wish to bring a pair of sunglasses to wear after the visit. One or more tests may need to be performed to help your treating physician assess the retina and macula (the central portion of the retina).
Retina conditions Pepose Vision treats
Treating retina conditions is a very specialized practice within the field of opthalmology. Pepose Vision is proud to be a leader in retinal services, and treats patients with a wide variety retinal conditions including the following.
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is the leading cause of vision loss in the U.S., affecting individuals 50 years of age or older. As the baby boomers age, the disease is becoming a significant problem. The disease affects the part of the retina called the macula, which is responsible for central vision. Even though macular degeneration can cause visual impairment, the disease usually does not cause peripheral vision loss or lead to total blindness.
Types of Macular Degeneration

The two common types of macular degeneration are “dry” and “wet.”
“Dry” form – the most common form of macular degeneration is caused by aging and thinning of the tissues in the macula. It develops slowly and usually causes mild vision loss. As this form of the disease develops, people often notice a dimming of vision while reading.
“Wet” form – rare, and more severe. Wet AMD is less common than dry AMD, but with the potential to create a large blind spot in the center of the visual field. Wet AMD can progress rapidly, potentially leading to legal blindness.
The causes of macular degeneration are not completely understood, but there is a strong hereditary component. Genetic testing is available at the Pepose Vision Institute.
Symptoms of Macular Degeneration
- A dark area in the center of vision
- Blurred or wavy vision
- Distortion
Treatment of Macular Degeneration
“Dry” form – There is no treatment for dry macular degeneration. Low vision aids can help maintain an excellent quality of life for those with visual impairment. High dose antioxidant vitamin therapy may slow the progression of disease in patients with moderate or severe disease. Anti-oxidant vitamins have not been shown to be beneficial for patients with no macular degeneration or early macular degeneration.
“Wet” form – a variety of therapies are available for wet macular degeneration. Intravitreal injections are the standard of care, with photodynamic therapy and laser photocoagulation rarely used.
Please visit our Age-Related Macular Degeneration page to learn more.
Central Serous Retinopathy
Central serous retinopathy is a disease that causes fluid to build up in the retina. This fluid leaks from blood vessels around the retina.
Symptoms
- Dim or blurred spot in the center of vision
- Distortion of straight lines
- Objects appearing farther away
Diabetic Macular Edema
Diabetic macular edema causes blurred vision when the macula swells from fluid leaking from the blood vessels around the retina.
Diabetic Retinopathy
The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the eyes. This damage may lead to diabetic retinopathy.
Types of Diabetic Retinopathy
Background or nonproliferative diabetic retinopathy – blood vessels in the retina are damaged and can leak fluid or bleed. This causes the retina to swell and form deposits called exudates. Many patients may not notice any change in their vision when they develop the early form of the disease, but it can lead to other more serious forms of retinopathy that severely affect vision. Fluid collecting in the macula is called macular edema and may cause difficulty with reading and other close work.
Proliferative diabetic retinopathy – new, fragile blood vessels grow on the surface of the retina. These new blood vessels are called neovascularization, and can lead to serious vision problems, because the new vessels can break and bleed into the vitreous. When the vitreous becomes clouded with blood, light is prevented from passing through the eye to the retina. This can blur or distort vision and frequently causes sudden and severe loss of vision. The new blood vessels can also cause scar tissue to develop, which can pull the retina away from the back of the eye. This is known as retinal detachment, and can lead to blindness if untreated. In addition, abnormal blood vessels can grow on the iris (the colored part in the front of the eye), which can lead to severe glaucoma.
Treatment of Diabetic Retinopathy
Good control of diabetes with intensive management and control of blood sugar will delay, and possibly prevent, both the development and progression of diabetic retinopathy. Patients with diabetic retinopathy frequently need to have special photographs of the retina taken. This series of photos is called fluorescein angiography.
The type of retinopathy, as well as the patient’s general health and eye structure, will determine the kind of treatment needed and the type of anesthesia utilized, but these are common surgery options:
- Laser photocoagulation
- Vitrectomy surgery
- Pharmacotherapy
Please visit our Diabetic Retinopahy page to learn more.
Distortion
Distortion could indicate a problem in the macula, the center of the retina. If you close one eye and look at something straight, like the edge of a door, blinds on a window, or the grid shown below, you should not see distortion. It is important to check each eye independently.
The sudden onset of distortion in an elderly person could be due to macular degeneration. In a middle-aged person, distortion could be the result of a macular hole, a macular pucker, or macular edema. These are all conditions that would require diagnosis and treatment by Pepose Vision’s retina specialist.
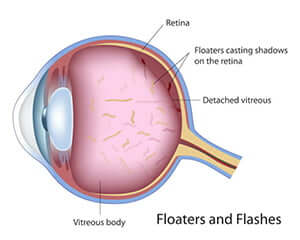
Floaters and Flashes
Floaters and Flashes may be a sign of normal aging of the vitreous gel, or the first sign of a retinal tear or detachment. At birth, the vitreous gel is 100% gel. The gel liquefies with age. As the gel liquefies, it pulls away from the surface of the retina. As the gel pulls, one may see a quick flash of linear, arc-shaped light off to the side. Eventually the gel pulls completely free, and there should be no problem. However, if the gel pulls hard enough, it may pull tissue from the surface of the retina, producing hair-like or fly-like images that migrate with eye movement. These are floaters.
If the vitreous tugs abnormally on the retina while it pulls away, it can tear the retina. If you experience flashes and/or floaters, you should be evaluated immediately since a torn retina can be repaired with an office procedure, avoiding the need for hospital surgery.
A torn retina can lead to a retinal detachment if the fluid inside the eye moves through the tear to enter the space behind the retina, lifting it off the back of the eye. A symptom of retinal detachment is the sudden onset of peripheral (off to the side) vision loss seen as a curtain or darkness. Retinal detachment always begins in the peripheral vision and progresses centrally. To preserve central vision, this condition must be promptly evaluated and treated at Pepose Vision Institute.
Macular Edema
Occurs when fluid and protein deposits build up on or under the macula and causes it to swell. The swelling may distort vision.
Macular Hole
A macular hole is a small break in the macula, located in the retina.
Macular Pucker
A macular pucker is scar tissue on the macula. It is caused by age or can be triggered by eye diseases or disorders such as detached retina, uveitis, or diabetic retinopathy.
Symptoms
- Blurry or Distorted Vision
- Difficulty seeing detail or fine print
- Gray area in center of vision
Plaquenil Toxicity
Side effects from the medication plaquenil (Hydroxychloroquine) may seriously effect the cornea and macula. Patients taking this medication are recommended to have regular exams, even when symptom-free.
Retinal Bleeding
Retinal bleeding can be caused by hypertension, a blockage of a retinal vein, or diabetes mellitus (which causes small fragile blood vessels to form, which are easily damaged). Retinal bleeding that take place outside of the macula can go undetected for many years, and may sometimes only be picked up when the eye is examined in detail with an ophthalmoscope.
Retinal Tear and Detachment
What is a retinal detachment?
As the vitreous gel in the back of the eye starts to liquefy, it can separate from the retina, a condition called vitreous detachment. If the vitreous gel adheres too firmly to the retina, a retinal tear can occur with a vitreous detachment. A retinal detachment occurs when fluid leaks through the tear and separates the retina from the back of the eye.
Symptoms of Retinal Tears and Detachments
Patients with retinal tear or detachment often, but not always, have flashes and floaters as their first symptoms. This occurs as the vitreous gel detaches from the back of the eye. Other patients may have very few symptoms. Patients may describe a “curtain” being drawn across the peripheral vision or decreased peripheral vision. If untreated, most retinal detachments will cause progressive loss of vision and eventually total blindness.
Treatment of Retinal Tears and Detachments
In most instances, retinal tears are treated with laser photocoagulation which acts to “spot weld” the retina to the back of the eye. In some cases pneumatic retinopexy is used to treat retinal detachment in the office without the need of surgery. In most cases, however, surgery is usually required. This consists of scleral buckling, vitrectomy, or a combination of the two procedures. These are usually performed as outpatient surgeries and may involve using a gas bubble to help push the retina back into position.
Retinal Vein Occlusion
Retinal vein occlusion is a blockage of the small veins that carry blood away from the retina.
Retinitis Pigmentosa
Retinitis pigmentosa is a group of genetic eye conditions that leads to incurable blindness. The condition starts with tunnel vision and is generally followed by night blindness, then legal blindness. Most will retain some sight all their lives, but some childhood cases causes total blindness.
Uveitis
Inflammation of the middle layer of the eye. It is estimated to be responsible for 10% of blindness in US patients.
Vitrectomy
A surgical procedure to remove some or all of the vitreous humor from the eye.
Vitreous Detachment
A condition of the eye in which the vitreous humour separates from the retina.
Frequently asked questions
Patient Testimonials
I just wanted to let you know how much we still appreciate the fabulous work you did for Adam and I. Adam is a Sr. and will graduate May 19. He is #18 out of 350ish. He will attend the Univ. of Missouri and enter the Pre-Veterinary Medicine Scholars program. After finishing sixty hours he can enter vet school. He’s also very active in FFA. Without the surgery you did I don’t know that any of this would have been possible!
He would still be the same young man but achieving the goals he sets for himself would have been a lot harder if he couldn’t drive and see as well as he does.
Again thank you and may God shine His blessings down on you and yours.
-Gratefully, Marsha Birk
Thank you for the care, expert medical treatment, and concern you have provided me. Without your medical intervention, I would not have experienced the greatest joy of my life – seeing the face of my grandbaby. Kalynn Erin and my family thank you too!
-Renee M
I just wanted to take this moment to thank you sincerely for my Vitrectomy surgery success, locating the problems with the retina in that eye as well, the healing process and follow-up guidance. In addition, for the findings today of the other eye’s retina tears and I Iook forward to Thursday when I get through the in-office procedure to remedy as well.
Also, I cannot say enough about the team in your surgery center as I had the Vitrectomy. The nurses and the anesthesiologist were so good to me and likewise, made the experience more comfortable than I imagined could be.
As you know, the best advertisement is a good recommendation and I have been doing that to friends. I highly recommend the Pepose Vision Institute.
-Sincerely, Cindy Z
What’s your next step?
If you’ve been diagnosed by your eye doctor with a retinal disease, or think you might have one of the symptoms, please come see us right away. Our experienced doctors will use advanced diagnostics to determine exactly how to help you see your very best, patiently answer your questions and carefully explain all your options.

