Corneal Transplants
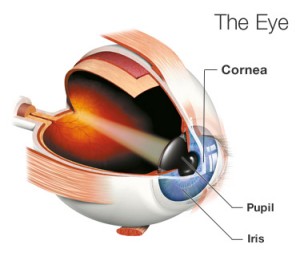
The cornea is the clear tissue covering the front of your eye. Like the crystal on your watch, your cornea serves as a protective window that allows light to enter your eye and come to focus on your retina. The cornea must remain clear for you to have good vision.
Corneal disease, degeneration or scarring from injury can cause the cornea to become cloudy and blur your vision. If corneal problems make it hard for you to see well enough to perform normal activities, such as reading or driving, a corneal transplant might help restore your vision.
A cornea transplant is a surgical procedure to replace part of your cornea with corneal tissue from a donor. A cornea transplant can restore vision,
reduce pain and improve the appearance of a damaged or diseased cornea. Also called keratoplasty, is typically performed as an outpatient procedure.
The doctors at Pepose Vision Institute are leading cornea specialists and have an excellent track record in corneal transplants. This translates into:
- Faster visual recovery: little to no discomfort
- Less need for repeat surgery to achieve best vision result possible
- Minimized risk of complications and transplant rejection that can compromise your sight
- The greatest amount of functional vision possible in the treated eye
When is a corneal transplant needed?
A corneal transplant is typically needed when:
- Vision cannot be corrected satisfactorily using other medical approaches
- Painful swelling cannot be relieved by medications or special contact lenses
- Corneal failure occurs after other eye surgery, such as cataract surgery
- Severe Keratoconus, a steep curving of the cornea, develops
- Hereditary corneal failure, such as Fuchs’ dystrophy, exists
- Scarring after infections, especially after herpes, occurs
- Rejection occurs after first corneal transplant
- Scarring arises after injury
Only an experienced, cornea subspecialty trained surgeon can appropriately determine if and when a transplant will enhance the quality of your vision.
We always provide our patients with compassionate and customized care.
How is a corneal transplant performed?
A cornea transplant is performed under local or general anesthesia at an outpatient surgery center. When we use local anesthesia, you may be able to hear what is going on, even though your eye and face will be numb and you may be groggy. Our cornea subspecialty trained surgeon will remove the hazy part of your cornea and a clear cornea from a donor will be put in its place. Tiny stitches, about 1/3 the diameter of a human hair, are used to hold this tissue in place. The procedure usually lasts for to two hours, depending on whether any additional procedures are done to remedy other vision problems in the eye.
Frequently asked questions

Corneal Transplant Case Study: Little Caitlin Kuehling was born with a condition called Peter’s Anomaly – in which the corneas are cloudy and the iris is misshapen. Essentially, she was functionally blind. Dr. Pepose knew that of the 40,000 cornea transplant operations in the country at the time, only 300 had been performed on babies. It was a risky procedure for an eye so small. But Caitlin’s mother Monica just wanted for her baby what other children had: “To see the moon and the stars and more.” It’s been more than 16 years since her operation, and that’s just what “Baby” Caitlin can now see. The moon. The stars. And all the beauty the world has to offer.
Why choose Pepose Vision for your corneal transplant surgery?
The eye doctors of Pepose Vision Institute have one of the best track records of protecting and restoring our patients’ functional vision of any cornea specialist in the country.
This translates into:
- Faster visual recovery: little to no discomfort.
- Less need for repeat surgery to achieve best vision result possible.
- Minimized risk of complications and transplant rejection that can compromise your sight of functional vision possible in their treated eye.
Experience
Cornea surgery outcomes improve dramatically if the surgeon is cornea subspecialty trained. It’s important to know that only cornea subspecialists at Pepose Vision Institute will perform your cornea procedure. Dr. Jay Pepose was recruited to Washington University/Barnes Hospital almost two decades ago because of his skill, training and experience in treating cornea-related injuries and disease.
Testing
Each cornea patient undergoes an intensive state-of-the-art testing process, directly supervised by our cornea subspecialty trained surgeons who then create a precise, personalized treatment plan.
Technology
Pepose Vision is always at the forefront of ophthalmic technology. As a research center, we often have access to technologies before most anyone else. We are leaders, both locally and nationally, in corneal tissue procurement and evaluation, relying on our state-of-the-art technologies to make sure that the donor tissue is safe and reduce risk of rejection.
Lifetime Commitment
Our surgeons vigilantly monitor the status of your eyes for the rest of your life to ensure that your vision continues to be its best, years AFTER your cornea surgery.
We recommend that the best way to ensure a successful outcome to your corneal transplant is to choose a highly experienced surgeon who is involved in developing state-of-the-art treatments to enhance your vision outcome.
Corneal Technology Leadership
Dr. Jay Pepose is one of the foremost cornea-subspecialty trained surgeons in the region and across the country. He has done pioneering work on tissue rejection and has served as Medical Director of MidAmerica Tissuebank Services, located in St. Louis. Dr. Pepose has performed thousands of corneal procedures, restoring and preserving the vision of infants, athletes and patients from all walks of life. The key to his success, and that of his team of cornea-trained surgeons, has been an uncanny ability to use the results of sophisticated diagnostic technologies to determine the appropriate surgical treatment for each cornea patient. Moreover, our cornea-trained surgeons are on-call 24/7, 365 days a year, so that any concerns can be addressed before they become major complications that threaten the initial transplant.
Because outstanding vision outcomes depend upon high-quality, precise preoperative analysis of your eyes, as well as advanced treatments and surgical techniques, we encourage you to learn more about:
Our State-Of-The-Art Diagnostic Tests
Our Advanced Treatement and Procedures
What’s your next step?
If you have any vision issues, please come see us.
Our experienced doctors will use advanced diagnostics to determine exactly how to help you see your very best, patiently answer your questions and carefully explain all of your options.


